Dr. Rachel McCardel
Despite the known benefits of breastfeeding, many mothers who work full-time can find it difficult, if not impossible, to continue breastfeeding after returning to work. Much of this, it turns out, boils down to lack of access – to information, space, time, privacy, fridges and more.
Rachel McCardel has focused her dissertation research on understanding the barriers to breastfeeding women face when they return to work, and she offers ways that organizations and individuals can improve access to important resources that mothers need to continue breastfeeding.
What do we know about how workplace breastfeeding policies are implemented?
First, we know access to workplace breastfeeding resources and policies varies by industry. For example, women working in management or professional occupations are more likely to have access to a private space to breastfeed at work and flexible break times for breastfeeding compared to women working in health care, education, and service or retail occupations. And, we know the following factors influence employers’ decisions about implementing breastfeeding policies: the presence of federal and state laws for breastfeeding mothers, organizational cultures that support breastfeeding, and having resources available to develop and implement policies for breastfeeding. From previous research, we learned that leadership support is a key facilitator for the implementation of wellness policies for employees, including breastfeeding support.
What legal protections are in place for breastfeeding women at work?
In the past 10 to 15 years, several federal protections have been implemented to support breastfeeding mothers in workplace settings. In 2010, The Patient Protection and Affordable Care Act (ACA) mandated that employers provide a private space, other than a restroom, and “reasonable” break times for employees to express breast milk during the workday, and health insurance companies were mandated to expand benefits to cover the costs related to breastfeeding supplies like breast pumps, as well as support and education from providers, such as lactation consultants. However, ACA provisions did not cover all breastfeeding employees. For example, federal provisions did not apply to worksites with fewer than 50 employees. In addition, not all insurance plans follow the ACA guidelines for breastfeeding supplies and support. Health insurance plans and policies that were implemented before 2013, those that were “grandfathered” in, are exempt from these requirements. In 2022, the Providing Urgent Maternal Protections for Nursing Mothers Act (PUMP Act) closed some of these loopholes. Under this law, nearly all breastfeeding employees are entitled to these resources except for employees who work in airline or railroad carriers, but employers with fewer than 50 employees can still receive an exemption from providing resources.
In addition to federal protections, many state governments adopted additional regulations to support breastfeeding employees, but these protections vary.
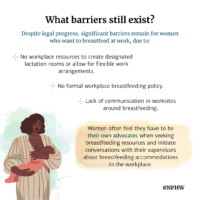
Why do you believe workplaces hesitate to implement breastfeeding policies? What barriers exist?
In my research, we found that employees working in a large worksite structure with several independent locations faced challenges with developing policies that were equitable and accessible to all employees in their organization. We also found that gaps exist in communication about breastfeeding policies in worksite settings. Women felt they had to be their own advocates when seeking breastfeeding resources and initiate conversations with their supervisors about breastfeeding accommodations in the workplace. They received very little information from their employers about the breastfeeding resources available in their organization and often needed to know if there was a formal breastfeeding policy in place.
Employers are hesitant to implement breastfeeding policies in worksite settings largely due to lack of resources available – time, budget, space – to provide permanent breastfeeding accommodations such as designated lactation rooms and flexible work arrangements. I also think there is a perception among employers that breastfeeding employees only need these resources for a limited time and this experience only affects a small number of employees within an organization. So, employers may think written policies are not needed if breastfeeding employees’ needs are being met and employers are fulfilling the requirements outlined in federal and state laws.
How do these policies intersect with maternity leave policies?
Maternity leave is a critical time for working mothers to physically recover after childbirth, adjust to new parenting responsibilities (such as breastfeeding), and prepare for their return to work. We know that working mothers who have longer lengths of maternity leave (i.e., more than 12 weeks) are more likely to continue breastfeeding after returning to work. However, there are gaps in access to paid maternity leave and women often face financial pressures to return to work earlier than 12 weeks. First, there is no federal policy in place to provide paid paternity leave to working parents. Instead, the Family and Medical Leave Act (FMLA) provides employees up to 12 weeks of unpaid leave to give birth and care for their infant. However, not every working mother is eligible for maternity leave under FMLA or can afford to take 12 weeks of unpaid leave. To fill these gaps, it is critical for states and employers to implement polices to provide paid paternity leave to all working parents and breastfeeding mothers.
How can employers better support breastfeeding?
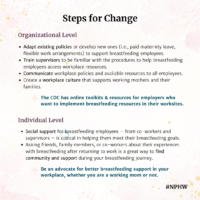
The CDC has online toolkits and resources for employers who want to learn more about breastfeeding support and how to implement breastfeeding resources in their worksites. At the interpersonal level, communication is key. Employers must communicate their policies to all employees within an organization to ensure everyone is familiar with the available resources. In addition, trainings are needed to ensure supervisors are familiar with the procedures to help breastfeeding employees access workplace resources and successfully return to work after giving birth. Employers can adapt existing workplace policies or develop new policies, such as paid maternity leave and flexible work arrangements, to support breastfeeding employees. Ultimately, creating an organizational culture that supports working mothers and their families is critical to increase support for breastfeeding, eliminate the barriers women face when accessing workplace breastfeeding resources, and alleviate the discomfort women often feel when asking for breastfeeding accommodations.
How can people who want to breastfeed advocate for themselves?
There are great resources available online – CDC, Office of Women’s Health, Mamava are a few – that explain the federal and state protections for breastfeeding mothers and provide strategies for working mothers to use when talking to their supervisors about breastfeeding accommodations at work. Finding social support for breastfeeding mothers is also critical in helping them meet their breastfeeding goals. Asking friends, family members, or coworkers about their experiences with breastfeeding after returning to work is a great way to share experiences and find resources to support your breastfeeding journey.
Infographics created by Emily Loedding.
Posted April 5, 2023.