How UGA’s Institute for Disaster Management is keeping Georgia’s nursing homes safe.
Curt Harris doesn’t care for the word, “No.” In his mind, it is often a barrier to progress. “No” shuts down cooperation and stifles creative thought.
As the director of the University of Georgia College of Public Health’s Institute for Disaster Management (IDM), Harris has worked to build a culture that is grounded by a can-do attitude that motivates IDM’s faculty, staff and students to work to find a way.
“The worst thing we can be told is ‘no,’ but ‘no’ for me is never ‘no,’” Harris said. “‘No’ just means I’ll figure out another way, but we’ll get there eventually.”
This philosophy has served IDM well throughout the past decade as they’ve led a series of grants, projects and initiatives supporting Georgia’s long-term care facilities to prepare and respond to a variety of emergencies and disasters.
 In many states, 2024 has brought record-breaking heat, massive storms and flooding events, and when these events cut out power, long-term care residents are particularly vulnerable.
In many states, 2024 has brought record-breaking heat, massive storms and flooding events, and when these events cut out power, long-term care residents are particularly vulnerable.
In 2016, the Centers for Medicare and Medicaid Services released Appendix Z, which required long-term care facilities (LTCs) to develop a program showing how they will keep residents safe during a disaster and how their preparedness efforts will plug into community-level emergency response plans.
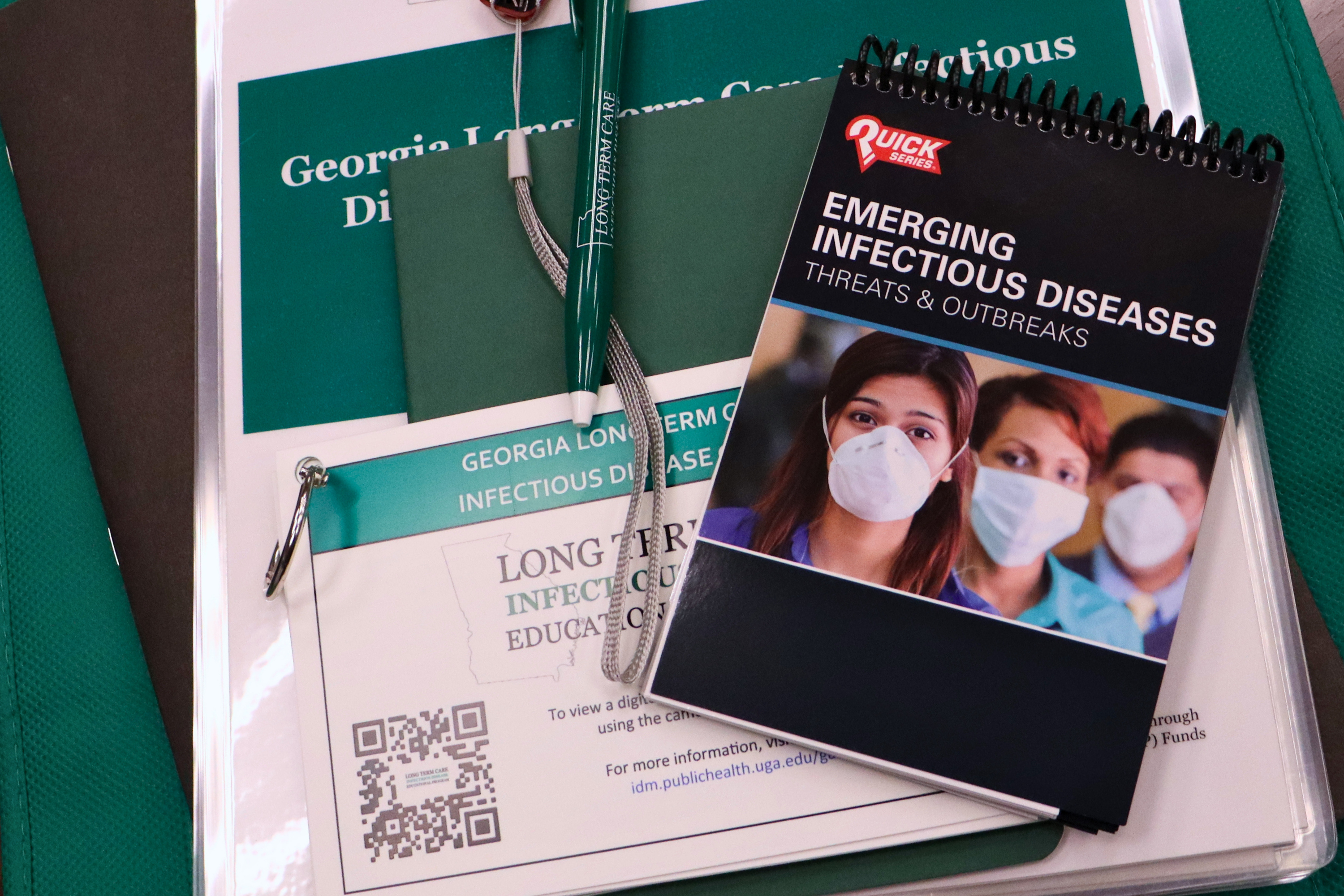
The Institute for Disaster Management provides trainings and resources for long-term care facilities, helping prepare and respond to emergencies ranging from diseases to natural disasters.
The change was meant to keep nursing home residents safe, but the change came with little support on how LTCs were to go about meeting these new requirements. The immediate aftermath of the policy change was dominated by confusion, concern and a little bit of chaos.
“They went from only having to have an evacuation plan and doing a fire drill to the floodgates opening,” Harris said. “When Appendix Z came out, these facilities received no education, no funding, and no personnel to help them do this.”
Since the 2010s, IDM had been slowly building relationships with LTCs in Georgia, working with facilities and organizations like the Georgia Health Care Association, the state’s largest association of long-term and post-acute health care providers, to align trainings, achieve regulatory compliance and drive better outcomes.
So, the Institute was well poised to help facilities all over the state meet new regulatory requirements with regard to their emergency and disaster readiness. With funding from CMS Civil Money Penalty Funds, they developed a program to educate skilled nursing facilities in Georgia on how to comply with Appendix Z.
“They saw an opportunity to try and help these facilities get their arms around these unbelievable regulations that you had to have in place all of a sudden,” said Susie Fussell, vice president for resident safety and emergency management with Magnolia Manor.
“It outlined the components you needed to have, the drills you had to do and all of that. In 2016, people were really struggling with how to be compliant,” Fussell added.
The COVID-19 pandemic briefly paused these efforts, but the find-a-way spirit instilled in the culture of IDM allowed them to quickly adjust. In-person training shifted to virtual with 83 percent of Georgia’s nursing homes participating in the program, while a separate grant that supported a similar program in South Carolina reached 74 percent of its nursing homes.
Furthermore, the financial savings achieved from going online for these sessions were then repurposed to create 340 emergency preparedness “go kits” filled with various tools and supplies that could be used in a crisis which were then delivered to participating Georgia nursing homes.
“I care that these facilities are safe, and I care that they are protecting the residents, the staff and the families,” Harris said. “By satisfying their requirements and becoming compliant, that’s the cherry on top for us.”
Establishing Trust
Crucial to the success of IDM’s initiatives is showing respect and listening to the needs of the LTCs they serve—that includes facility leaders and each staff member who has a role to play in carrying out the facility’s emergency plan.
“Often, a maintenance director at a nursing home has never been asked for their opinion on how the facility should respond to or prepare for a disaster,” said Alyssa Ragan, an emergency preparedness manager at IDM. “When they realize they have an important role to play, it’s a significant culture shift. It encourages everyone to get involved, and that involvement can save lives.”
Fussell says she can tell Harris and his team really internalize what they hear.

“They’ll think, ‘You know, what can we do to be a part of the solution?’ A lot of times they would call me just to ask, ‘Are we on the right track?’” she said.
So, it’s no surprise that when IDM team members kept hearing the frustrations voiced by colleagues in the long-term care community about the high turnover among Certified Nursing Assistants (CNAs), they sought to address it.
“They work in all kinds of settings all across the health care field, but they are especially important in longterm care and nursing homes in particular. They serve as really a backbone of that workforce,” said IDM emergency preparedness manager Austin Dobbs.
Up to 70 percent of the workforce in nursing homes are CNAs, and they can administer up to 90 percent of the direct resident care in these facilities. The work is physically demanding and stressful, and working with residents who are struggling with medical issues like cancer or dementia takes an emotional toll.
COVID-19 exacerbated another layer of pressure, with CNAs feeling responsible for keeping residents and themselves safe. These stresses and anxieties weighed across the workforce, impacting the mental health of countless personnel on the frontline of care. As such, turnover among CNAs, which was already widespread, accelerated, and recruitment proved challenging.
High staffing turnover also created a seemingly endless cycle of training and retraining for IDM’s programs. New LTC facility staff that joined in January could be gone by April, taking with them the effort and energy invested in preparing them for their role in case of an emergency.
So, IDM secured funding focused on recruitment and retention of CNAs, embarking on a comprehensive, integrated marketing campaign that outlined the career pathways that existed for CNAs and provided a series of cash stipends that were awarded to CNAs at various stages of training and certification as an incentive.
Harris pointed out that several facilities that piloted the program for them are now close to being fully staffed.
“They understood how we were being crippled by not having enough staff to take care of our people, and we do have a staffing mandate,” Fussell said. “They realized the urgency, and they did have to really think outside the box. They made it happen, and that was fantastic.”
Success with each new initiative tends to produce new challenges, and IDM’s recruitment and retention efforts for CNAs are no exception.
Before becoming a CNA, candidates who graduate from a technical college must pass a written exam and conduct a skills evaluation. The written exam is relatively easy to access and can be taken at any time. The skills evaluation, however, was done in person and, prior to 2023, was run by a single provider. Aspiring CNAs could face up to 6 months of delays before they could start working at a facility, potentially driving them to a new job.
Once again looking to fix problems rather than accept them as inconvenient truths, Harris said his staff began to explore ways to increase access to the skill evaluation by making it virtual.
After some initial conversations with the Georgia Department of Community Health, IDM turned around a proposal to launch a virtual skills evaluation program for CNAs in April 2023 and conducted its first pilot evaluation just three months later.
“It was clear the scheduling of those skills and the availability of who were doing the skills check off was bogging down the system,” Fussell said. “At Magnolia Manor, we piloted the virtual skills assessment for CNAs, and it has been a tremendous success. We worked very closely with the leadership there at IDM and had many calls and emails back and forth about how this could be done appropriately.”
By August, the program was rolled out to the entire state, free of charge.
“I think th at’s what we all enjoy about working at IDM—every day is different and we’re always looking to the next thing,” Ragan said. “You’re continuously improving the project you’re on and that’s one of the big benefits from all of our trainings. It’s not something that is recorded, put online, and just sits there. We review feedback from every course and we’re updating things all the time.”
at’s what we all enjoy about working at IDM—every day is different and we’re always looking to the next thing,” Ragan said. “You’re continuously improving the project you’re on and that’s one of the big benefits from all of our trainings. It’s not something that is recorded, put online, and just sits there. We review feedback from every course and we’re updating things all the time.”
“Really, IDM’s culture of excellence is what makes all the programs we have so successful,” she said.
With disasters increasing in number and impact, the need to protect the health and safety of aging populations has never been more apparent. However, with a regulatory landscape in constant flux, providing the resources, trainings and planning needed for the facilities many older adults call home to thrive is paramount, and Harris knows his team will be ready.
“We’re in a constant state of flexibility—I don’t know what’s coming next, but I know IDM is in it, whatever it is,” Harris said.
By Johnathan McGinty
This article was first published in the 2024 issue of the UGA College of Public Health magazine.