New study measures how systemic inequality contributed to COVID-19 burden on Black communities in Georgia
The COVID-19 pandemic has disproportionately burdened communities of color across the U.S. By fall of 2020, Black, Latinx, and Indigenous communities were experiencing death rates that almost tripled those of White communities.
Now, new research from the University of Georgia shows how racialized economic inequalities drove poor outcomes for Black residents in Georgia.
Early reports on COVID-19 cases focused on individual risk factors, like having a chronic condition, which generally show up in higher rates in Black communities compared to other groups. But co-morbidities couldn’t fully explain the excess burden experts were seeing.
“And so that points us to things that are structural, which is proportionately high exposure and limited access to care,” said study author Amit Eichenbaum, who recently graduated from UGA’s dual-degree Doctor of Veterinary Medicine and Master of Public Health program.
“For example, African Americans are much more likely to work essential jobs, which have increased exposure because they can’t always be done from home. And these workers are less likely to have paid sick days, and they’re also significantly less likely to be insured.”
Eichenbaum worked with Allan Tate, an assistant professor of epidemiology and biostatistics at UGA’s College of Public Health, to better understand how structural factors contributed to COVID-19 burden in Georgia during the first eight months of the pandemic.
Quantifying Inequity

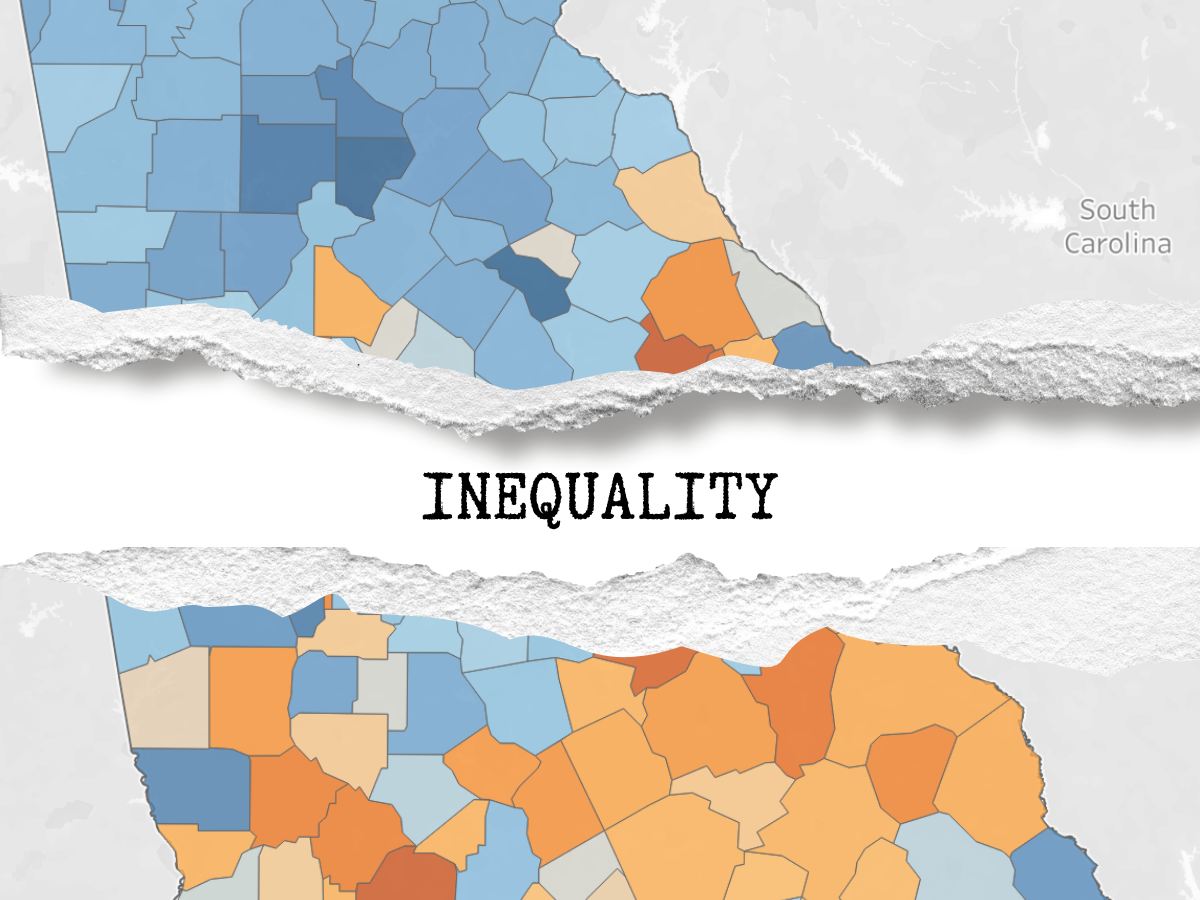
Heat Maps, Georgia Counties (n=159): Higher concentrations of deprivation indicated by the orange gradient. Higher concentrations of privilege indicated by the blue gradient. The combined ICE measure for race and income (high-income White-American vs. low-income Black American).
Their study used a metric to describe how historical and current inequities among Georgia counties were related to higher COVID-19 case rates, hospitalization and deaths in the first wave of the pandemic.
The Index of Concentration at the Extremes, or ICE, is a tool to help quantify how structural racism leads to poor health outcomes, based on attributes of where people live. Using county-level income and demographic data, the ICE metric shows how populations cluster into groups, some with more resources and others with less.
“Essentially it’s able to capture polarization,” said Eichenbaum. “Polarization is a lot more valuable in identifying and predicting negative health outcomes than, say, just looking at one area that is deprived in terms of income.”
ICE is particularly useful for capturing historical disparities that have persisted for decades or longer , says Tate, which isn’t reflected in income data alone.
Eichenbaum and Tate calculated ICE scores for income, race, and combined race and income for each of Georgia’s counties. The combined race and income ICE scores were then grouped into three categories of low to increasing socioeconomic privilege.
The researchers then analyzed these categories as predictors of COVID-19 case rates, hospitalizations and deaths observed through October 2020 to determine how strong of a relationship existed between privilege and disease burden.
The Burden of History
Counties that had the greatest racialized economic segregation, they found, saw 1.5 times the case rates and 1.7 times the death rate, and these counties had almost twice the case hospitalization rate.
“So, people in those counties that had COVID were almost twice as likely to have to be hospitalized, and of course that hospital burden affects everyone,” said Eichenbaum.
Critically, they found that the ICE scores for income alone were not as strongly associated with these outcomes.
“By chance of where people live, poor COVID outcomes may be a consequence of an inability to control one’s exposure to unsafe environments, especially during a pandemic when the privilege of being able to work from home or live in safer places was not accessible for everyone, based on income and work status,” said Tate.
“These data demonstrate why the incidence rate was elevated before there were large scale interventions, like systematic lockdowns or mask mandates.”
“There are better ways for us to identify where resources should be allocated, and it’s important to turn the conversation away from individual-level interventions to the more systemic and structural interventions. We should do the work now because we’re going to need it in the future,” said Eichenbaum.
– Lauren Baggett
Posted on April 21, 2022.